LOS ANGELES — As public health departments across the nation conduct testing for novel coronavirus, they’ve also begun conducting antibody tests — a move experts say could help officials determine how to redeploy the U.S. workforce and aid the development of a vaccine.
The number of positive coronavirus cases in the U.S. eclipsed 662,000 Friday and nearly 30,000 Americans have died, according to Johns Hopkins University data. Meanwhile, the Trump administration continues its push for a summer reopening of the economy.
An economic recovery would benefit some of the more nearly 27 million Americans out of work and struggling in an economy expected to contract 6% this year, according to an International Monetary Fund report which also predicts the global economy will shrink 3%.
But U.S. health officials and political leaders, including California Gov. Gavin Newsom, said this week any phased reopening of the economy must be guided by science and an understanding that a poorly planned restart could trigger mass infections.
Los Angeles County Public Health Department chief science officer Paul Simon told Courthouse News recovery plans must include safety measures to ensure workers won’t contract SARS-CoV-2 — the novel coronavirus that causes Covid-19 — or become infected again.
“We want to loosen things up as soon as possible, but we want to be careful because we could get another wave of infections that overwhelm hospitals,” Simon said, adding social-distancing measures stem potential case surges and give scientists time to develop a vaccine.
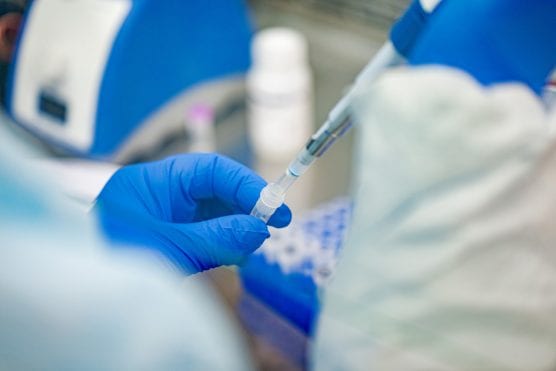
To better understand how the virus spread and how patients overcame infection, L.A. County partnered with University of Southern California researchers to look for antibodies in blood samples of 1,100 residents.
The serological test looks for immunoglobulin M (IgM) and immunoglobulin G (IgG) antibodies, proteins that help people fight off viral infections, Simon said.
“We think the study will give us a more complete picture of what the pandemic looks like,” Simon said regarding the serological test. “We’ve been primarily focused on people who’ve tested positive. What’s missing is people with mild symptoms or no symptoms who didn’t seek testing.”
Results from the roughly 900 samples collected last week will shed light on residents’ risk of hospitalization and the county’s true fatality rate, which Simon believes will be lower as more data comes in.
“We’re currently counting people that had COVID-19 and died, but the number of folks infected countywide is larger,” Simon said.
Simon said the test isn’t recommended for individual patient care since someone could have antibodies in their blood that cross-react with the testing kit.
Though the study targets a range of individuals across racial, economic and geographic differences, Simon said the study materials have not yet been translated into Spanish or other languages prevalent in the county.
Researchers plan to conduct a survey every three weeks with different sample groups in L.A. County, where 10,900 people have contracted the virus and 455 have died as of Thursday.
Los Angeles Mayor Eric Garcetti said in a public briefing Wednesday the serological testing will aid real-time identification of new COVID-19 cases as well as track hotspots where infections spike.
“These blood tests are the easiest way to see who has had the virus, but the test doesn’t speak to someone’s infectiousness,” Garcetti said, adding officials hope to make serological testing available on a mass scale.
This month, San Miguel County, Colorado, tested 986 people for antibodies, finding eight positive cases and 23 with “indeterminate” or borderline results.
Positive and borderline cases signal recent exposure and that someone is in the early stage of developing antibodies, officials said in a statement. They said the results are also treated as presumptively active infections.
Negative results could also mean someone was recently exposed but has not yet developed antibodies.
Plasma from people who’ve recovered from the COVID-19 infection could be used in treatments for those who’ve been infected with the virus.
Sharon Grundy, the San Miguel County medical officer, said officials are developing protocols for plasma donations from people with positive results.
In L.A. County, residents interested in donating plasma can contact health officials to be connected to researchers though testing kits are currently in short supply, Simon said.
The National Institutes of Health said last week its plan to test 10,000 volunteers for antibodies will provide critical data since current molecular testing doesn’t determine whether a person was previously infected and recovered. People who have tested positive for the novel coronavirus or who currently have symptoms are not eligible to participate in the study.
Carol Shoshkes Reiss, biology and public health professor at New York University, told Courthouse News it’s common for health officials to use serological tests during virus outbreaks.
Reiss said the tests were vital in the fight against Ebola and Zika viruses and critical for vaccine development, which could be one or two years away for the novel coronavirus.
But tests won’t determine if someone who was once infected is now immune, though antibodies can be re-stimulated with new exposure to the COVID-19 virus, Reiss said.
Tests will also show whether the virus was present earlier in communities, including as far back as December when flu-like symptoms may not have been immediately recognized as COVID-19-related, Reiss said.
“What we know about the spread of the virus is that many people are asymptomatic,” Reiss said. “Meaning they’ve had exposure — not just to someone who’s sick but to the infection to some degree — and were able to recover without serious symptoms.”
Irving Steinberg, pharmacotherapeutics and infectious diseases expert at USC, said in an interview that antibody testing will help employers develop staffing plans based on the level of risk of virus exposure.
“The more people are immune or asymptomatic and develop antibodies, the more you know you can be safer around those people,” Steinberg said. “Especially if we go into the next season without a [COVID-19] vaccine, we will need to know what level of workers — especially health care — have durable immunity.”
The public could be asked to obtain certificates of immunity in order to re-enter a workforce built around strict health protocols, Steinberg said, adding the measures could result in exclusive behaviors if not crafted equitably.
“Will there be discrimination against folks who can’t develop an immunity response?” Steinberg asked.
Regarding LA County’s decision to not collect demographic data during antibody testing, Steinberg said the more that is known about the test subjects the better the response to the pandemic will be.
“That has to do with access to care,” Steinberg said. “[Demographic data] could demonstrate biases in the system or intrinsic problems. In terms of spread, if we know more, be it local or national, the better off we’ll be in investing resources.”
The spread of the virus has prompted stay-at-home orders in nearly every state, a key component in stemming the surge of infections. The tests will help officials determine whether those restrictions are working or if they’re not working well enough, said Steinberg.
The severity of the COVID-19 outbreak may motivate people to get tested more routinely — and vaccinated, once one is developed — and even embrace invasive tracking systems that identify points of contact with infected individuals, Steinberg said.
“Tracking people helps us understand if public health responses will require vaccines on an annual basis,” Steinberg said, adding that a vaccine would take more than a year to amplify and distribute nationwide. “If [COVID-19] reappears next season, will it mutate?”
— By Martin Macias Jr., CNS
Like this:
Like Loading...
Related



 Tweet This
Tweet This Facebook
Facebook Digg This
Digg This Bookmark
Bookmark Stumble
Stumble RSS
RSS
























REAL NAMES ONLY: All posters must use their real individual or business name. This applies equally to Twitter account holders who use a nickname.
0 Comments
You can be the first one to leave a comment.