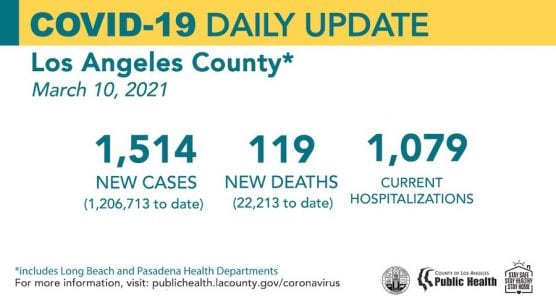
The Los Angeles County Department of Public Health confirmed Wednesday 119 new deaths and 1,514 new cases of COVID-19, with 26,666 total cases in the Santa Clarita Valley.
To date, Public Health identified 1,206,713 positive cases of COVID-19 across all areas of L.A. County and a total of 22,213 deaths. Cases reported Wednesday include a few hundred backlogged cases from faxed provider reports.
The seven-day average number of cases by episode date has decreased to less than 700 per day as of March 2.
As cases decline the numbers of people hospitalized for COVID-19 continue to decline, though we are not back to the pre-surge level. There are 1,079 people with COVID-19 currently hospitalized and 30% of these people are in the ICU.
Testing results are available for more than 5,915,000 individuals with 19% of people testing positive. Wednesday’s daily test positivity rate is 2.3%.
COVID-19 Variants
To date, Public Health has confirmed a total of 47 cases of COVID-19 U.K. variant, 9 cases of New York variant and one case of the P.2 Brazil variant in Los Angeles County. All the cases of the U.K. variant have been identified since Jan 15, and the first case of the P.2 variant from Brazil was identified two weeks ago. All 9 cases of the NY variant were identified since March 3. In addition, there have been 262 California variant cases identified, with the vast majority of these cases identified since December 1 of last year. There have been no cases identified in L.A. County with the South African variant. This latest analysis of specimens is the first time the New York variant was identified in Los Angeles County.
Of the 119 new deaths reported Wednesday, 44 people that passed away were over the age of 80, 33 people who died were between the ages of 65 and 79, 30 people who died were between the ages of 50 and 64, six people who died were between the ages of 30 and 49, and one person died who was between the age of 18 and 29. Five deaths were reported by the city of Long Beach.
California Wednesday Snapshot
Statewide, the California Department of Public Health confirmed Wednesday a total of 3,513,678, with 54,621 deaths from the disease. There are 3,625 confirmed hospitalizations and 992 ICU hospitalizations in California.
Numbers may not represent true day-over-day change as reporting of test results can be delayed.
There were 6,412 newly recorded confirmed cases Tuesday.*
The 7-day positivity rate is 2.4% and the 14-day positivity rate is 2.3%.
There have been 50,223,971 tests conducted in California. This represents an increase of 84,140 during the prior 24-hour reporting period.
As case numbers continue to rise in California, the total number of individuals who will have serious outcomes will also increase.
As of March 10, providers have reported administering a total of 10,772,859 vaccine doses statewide. The CDC reports that 14,650,550 doses have been delivered to entities within the state, and 15,107,575 vaccine doses, which includes the first and second dose, have been shipped. Numbers do not represent true day-to-day change as reporting may be delayed.
Health Care Worker Infection Rates
As of March 9, local health departments have reported 97,997 confirmed positive cases in health care workers and 409 deaths statewide.
Santa Clarita Valley Wednesday Update
As of 6:15 p.m. Wednesday, the L.A. County Public Health dashboard recorded 272 deaths among Santa Clarita Valley residents since the pandemic began.
The following is the community breakdown of the SCV residents who have died, according to the L.A. County dashboard:
233 lived in Santa Clarita
17 in Castaic
7 in Acton
3 in Agua Dulce
3 in unincorporated Canyon Country
3 in Stevenson Ranch
1 in unincorporated Bouquet Canyon
1 in Lake Hughes
1 in Newhall
1 in unincorporated Saugus/Canyon Country
1 in Val Verde
1 in Valencia
Of the 26,666 cases reported to Public Health for the SCV to date, the community breakdown is as follows:
City of Santa Clarita: 19,503
Castaic: 3,631
(includes Pitchess Detention Center and North County Correctional Facility*)
Stevenson Ranch: 1,083
Canyon Country (unincorporated portion): 803
Acton: 455
Val Verde: 318
Agua Dulce: 258
Valencia (unincorporated portion west of I-5): 184
Saugus (unincorporated portion): 132
Elizabeth Lake: 75
Newhall (Unincorporated portion): 66
Bouquet Canyon: 45
Lake Hughes: 40
Saugus/Canyon Country: 40
Sand Canyon: 17
San Francisquito/Bouquet Canyon: 15
Placerita Canyon: 1
*Note: The county is unable to break out separate numbers for Castaic and PDC/NCCF because the county uses geotagging software that cannot be changed at this time, according to officials. Click here for the LASD COVID-19 dashboard.
Henry Mayo Newhall Hospital Wednesday Update
Henry Mayo Newhall Hospital reported Wednesday no additional COVID-19 deaths, zero cases pending, six patients were hospitalized in a dedicated COVID-19 unit receiving ICU-level care, and a total of 1,171 patients had been treated and discharged, hospital spokesman Patrick Moody said.
Privacy laws prohibit the hospital from releasing the community of residence for patients who die there; that info is reported by the L.A. County Public Health COVID-19 dashboard, which generally lags 48 hours behind.
 L.A. County
L.A. County
Los Angeles County has now met the threshold to start qualifying for the State’s Blueprint for a Safer Economy less restrictive red tier that allows for additional re-openings. L.A. County’s adjusted case rate dropped from 7.2 new cases per 100,000 people to 5.2 new cases per 100,000 people. The test positivity rate dropped from 3.5% to 2.5%, and in areas with the fewest health affirming resources, L.A. County has a test positivity rate of 3.6%.
The County needs to have qualifying metrics for one more week to be eligible on March 17 for additional re-openings.
The County could move to the red tier sooner because the state has an acceleration trigger built into the Blueprint that allows counties to move to the red tier if their case rate is below 10 new cases per 100,000 residents once 2 million doses of vaccine have been administered to residents across the state living in the least resourced communities. Once this vaccination threshold is met L.A. County will qualify to move into the red tier since the County will have already had an adjusted case rate of under 10 new cases per 100,000 residents for two consecutive weeks. The state is reporting over 1.9 million vaccines have been administered to date to residents in under-resourced communities. Given all the efforts this week to make sure people in the hard-hit communities have better access to vaccines, it may only be a couple of days until the 2 million threshold is reached.
Public Health continues to work with the Board of Supervisors and sector partners to prepare modifications to the Health Officer Order to permit additional activities allowed in the red tier. L.A. County schools will be able to open on-site learning for grades 7 through 12 once the County moves into the red tier. One effective strategy for reducing the risk of transmission of COVID-19 is for schools to create stable learning groups. A stable learning group is a fixed group of students and staff that stays together minimizing any mixing with any other groups for any activities. Creating and maintaining stable groups is required for students attending in person instruction in grades TK through 6 and strongly recommended for in-person learning for students in grades 7 through 12. Schools all need to maintain distancing, masking and infection control practices for re-openings to happen with as much safety as possible. While vaccinations and testing are additional available tools, they are not a substitute for core public health practices that, when used with fidelity, significantly limit virus transmission.
“(Wednesday) marks the one-year anniversary of the first death from COVID-19 here in L.A. County. Tragically, one year later, over 22,000 people, including grandparents, mothers and fathers, sisters and brothers, friends and co-workers, have passed away from this terrible virus here in L.A. County, leaving a huge void behind. There has been tremendous tragedy and suffering here and across the world, and to all who are mourning, we are with you in your sorrow,” said Barbara Ferrer, PhD, MPH, MEd, Director of Public Health. “Variants remain a concern, even as more and more people are vaccinated. As we plan for additional re-openings, we know that if there is more transmission of the COVID-19, there is more risk of variants dominating and more risk of suffering. That is why it is so important for all of us to continue to do everything we can to reduce transmission, including masking and maintaining physical distance whenever we are outside of our homes and around others.”
Custodians and janitors, public transit workers, and airport ground crew workers are all now eligible to be vaccinated, as directed by the State. Emergency responders like social workers who handle cases of violence, abuse or neglect and foster parents providing emergency housing for young people, are also eligible to be vaccinated. We are currently coordinating with unions and employers to set up vaccination sites and make appointments at our large county sites available for these groups. For the janitorial and custodial workers, we are in the process of creating appointments this weekend on both Saturday and Sunday at the Forum and on Saturday at the LACOE/Downey vaccination site.
Next week, on Monday, March 15, vaccine eligibility will open up to people ages 16 through 64 who have underlying health conditions or disabilities that put them at the highest risk of becoming very sick from COVID-19. These conditions include:
– Cancer, with a current weakened immune system
– Chronic kidney disease, stage 4 or above
– Chronic pulmonary disease, oxygen dependent
– Down syndrome
– Solid organ transplant, leading to a weakened immune system
– Pregnancy
– Sickle cell disease
– Heart conditions, such as heart failure, coronary artery disease, or cardiomyopathies (but not hypertension)
– Severe obesity with a BMI of more than 40
– Type 2 diabetes with A1c level greater than 7.5%
– Or Having a disability that: makes serious illness from COVID-19 likely; would, if positive for COVID-19, limit the person’s ability to received care vital to their well-being and survival; or would make the treatment for COVID-19 particularly challenging.
Providers and healthcare facilities are working to use their health record systems to identify patients who have these conditions and reach out to them so they can be vaccinated. It is our understanding that the state will be releasing guidance on other ways people with these conditions can verify their eligibility to be vaccinated.
Throughout the pandemic, people living in low-resourced neighborhoods and people of color have been disproportionally impacted by COVID-19. While we see cases dropping overall, there remains a gap between Latino/Latinx residents and other groups, though this gap is narrowing. The rate dropped from a peak of 2,452 new cases per 100,000 people in early January for Latino/Latinx residents to 139 new cases per 100,000 people as of February 27. Black/African American residents have the second highest case rate of 78 new cases per 100,000 people. White residents have a case rate of 73 new cases per 100,000 people and Asian residents have a case rate of 63 new cases per 100,000 people.
When the surge began in early- November, the average number of Latino/Latinx residents who passed away each day was 3.4 deaths per 100,000 people and then sharply increased to 59 deaths per 100,000 people in mid-January. As of February 27, the mortality rate among Latino/Latinx residents has declined to 13 deaths per 100,000 people, yet still remains more than double that of other groups. Since mid-January, the mortality rate among African American/Black residents decreased from nearly 29 deaths per 100,000 people to 6 deaths per 100,000 people. Deaths among Asian residents have declined since the peak, from 26 deaths per 100,000 people to 5 deaths per 100,000 people. The current mortality rate among White residents is also 5 deaths per 100,000 from the peak of about 20 deaths per 100,000.
In mid-January, those in the lowest resourced areas were experiencing an average of 70 deaths each day from COVID-19 per 100,000 residents. That was more than three times the death rate for those living in higher income areas at 22 deaths per 100,000 people. As of February 27, the mortality rate among residents in the lowest resourced areas decreased to 12 deaths from COVID-19 per 100,000 people, twice that for people living the highest resourced areas, at 6 deaths per 100,000 people. The gaps are closing, just not as quickly as we would like.
As we vaccinate our residents who are 65 and older, we are seeing a very similar and damaging pattern of disproportionality. White and Asian residents 65 and older continue to have the highest vaccination rate. As of March 6, almost 59% of White residents and almost 53% of Asian residents 65 and older have received at least one dose of the vaccine. Almost 48% of American Indian/Alaska Native residents, 43% of Latinx residents, and 38% of Black residents who are age 65 and older have received at least one dose. While these inequities are stark and unfair, we are working to close these gaps and have made some progress improving vaccination rates in the hardest hit communities. The vaccination rate for Black residents saw the largest increase at almost 92%. For American Indian/Alaska Native residents, the vaccine rate increased almost 70%, and for Latinx residents the vaccine rate increased by 65.8%. The vaccine rate for White residents increased by 46.1% and for Asian residents increased 44.3%.
As more groups become eligible to be vaccinated and we continue to have a shortage of supply, we are prioritizing closing these gaps and making sure that the hardest hit communities have access to the vaccine and barriers that prevent this are mitigated. Strategies to ensure this include: having sites in areas that have been most impacted by this pandemic and have the fewest resources; collaborating with faith based and community based partners to make appointments for community residents, and creating ways to solve transportation and registration barriers. We will continue to work with our extraordinary partners to innovate and create ways that are tailored to our county and to the people who live here so that everyone has access to the vaccine.
For information about vaccine appointments in L.A. County and when your turn is coming up, to sign up for a vaccination newsletter, and much more, visit www.VaccinateLACounty.com (English) and www.VacunateLosAngeles.com (Spanish).
The Reopening Protocols, COVID-19 Surveillance Interactive Dashboard, Roadmap to Recovery, Recovery Dashboard, and additional things you can do to protect yourself, your family and your community are on the Public Health website, www.publichealth.lacounty.gov.
California Wednesday

***Note: The statewide case count includes 4558 confirmed COVID-19 cases reported by Los Angeles County. Of these, 880 were newly identified cases. The remaining 3678 cases reported on 3/9 were cases that were previously identified as probable between July 14, 2020 and March 7, 2021 and were reclassified as confirmed cases.
Tracking Variants
Multiple variants of the virus that causes COVID-19 have been identified globally during the COVID-19 pandemic. These genetic mutations are expected, and some emerge and then disappear, while others persist or become common. Most variants do not have a meaningful impact. Public health becomes concerned about a variant when it affects COVID-19 transmission, severity, testing, treatment or vaccine effectiveness. Get more information on the variants CDPH is currently monitoring.
Blueprint for a Safer Economy
With the Regional Stay at Home Order rescinded statewide as of Jan. 25, all counties are now under the rules and framework of the Blueprint for a Safer Economy and color-coded tiers that indicate which activities and businesses are open based on local case rates and test positivity.
Blueprint Summary as of March 9
34 counties in the Purple (widespread) Tier
20 counties in the Red (substantial) Tier
3 counties in Orange (moderate) Tier
1 county in the Yellow (minimal) Tier
Blueprint tiers are updated weekly on Tuesdays. Find the status of activities in specific counties.
Additional Date and Updates
County Map – Local data, including tier status and ICU capacity
Data and Tools – Models and dashboards for researchers, scientists and the public
Blueprint for a Safer Economy – Data for establishing tier status
Updated Travel Advisory
CDPH has issued an updated travel advisory. Postponing travel and staying home is the best way to protect yourself and others from COVID-19. Non-essential travelers from other states or countries are strongly discouraged from entering California and should adhere to the state’s self-quarantine procedures for 10 days.
Safe Schools for All Plan
Gov. Newsom released his California’s Safe Schools for All plan, California’s framework to support schools to continue operating safely in person and to expand the number of schools safely resuming in-person instruction.
Vaccinate All 58
The COVID-19 shipment of the COVID-19 vaccine has arrived in California, and additional shipments will continue to arrive throughout this week. The first doses are being administered to health care workers and residents of long-term care facilities. The state is working closely with community partners and stakeholders to help ensure the vaccine is distributed and administered equitably across California. For more information, visit the CDPH COVID-19 Vaccine webpage and Vaccinate All 58.
New Testing Turnaround Time Dashboard
The testing turnaround dashboard reports how long California patients are waiting for COVID-19 test results. California has worked to reduce testing turnaround times in recent weeks to help curb the spread of the virus. During the week of Feb. 21 – Feb. 27, the average time patients waited for test results was 1.2 days. During this same time period, 78% of patients received test results in one day and 94% received them within two days.
Data and Tools
A wide range of data and analysis guides California’s response to COVID-19. The state is making the data and its analytical tools available to researchers, scientists and the public at covid19.ca.gov.
Multisystem Inflammatory Syndrome in Children (MIS-C)
As of March 8, 357 cases Multisystem Inflammatory Syndrome in Children (MIS-C) have been reported statewide. MIS-C is a rare inflammatory condition associated with COVID-19 that can damage multiple organ systems. MIS-C can require hospitalization and be life threatening.
MIS-C is a rare inflammatory condition associated with COVID-19 that can damage multiple organ systems. MIS-C can require hospitalization and be life threatening. Parents should be aware of the signs and symptoms of MIS-C including fever that does not go away, abdominal pain, vomiting, diarrhea, neck pain, rash, bloodshot eyes or feeling tired. Contact your child’s doctor immediately if your child has these symptoms. Early diagnosis and treatment of patients is critical to preventing long-term complications.
New Health Equity Dashboard
The COVID-19 pandemic has highlighted existing inequities in health that are the result of structural racism and poverty, and the disproportionate prevalence of underlying conditions such as asthma and heart disease among Latinos and African Americans. As part of its commitment to reduce health inequities and ensure the best outcomes for all Californians, the state has launched a Health Equity Dashboard on www.covid19.ca.gov. View COVID-19 Race & Ethnicity Data and Cases and Deaths by Age Group.
Popular links include:
– The Statewide COVID-19 Dashboard
– The California COVID-19 Assessment Tool (CalCAT)
– State Cases and Deaths Associated with COVID-19 by Age Group
– COVID-19 Race & Ethnicity Data
– COVID-19 Hospital Data and Case Statistics
– View additional datasets at the California Open Data Portal (Including: Testing Data, PPE Logistics Data, Hospital Data, Homeless Impact and more)
Your Actions Save Lives
California is experiencing the fastest increase in cases we have seen yet – faster than what we experienced at the outset of the pandemic and this summer. If COVID-19 continues to spread at this rate, it could quickly overwhelm our health care system and lead to catastrophic outcomes. Protect yourself, family, friends and community by following these prevention measures:
– Staying home except for essential needs/activities and following local and state public health guidelines when visiting businesses that are open.
– Following the Limited Stay at Home Order that requires allnon-essential work and activities to stop between 10 p.m. and 5 a.m. in counties in the purple tier. The order took effect at 10 p.m. Saturday, November 21, and will remain in effect until 5 a.m. December 21.
– Staying close to home, avoiding non-essential travel, and practicing self-quarantine for 14 days after arrival if you leave the state.
– Keeping gatherings small, short and outdoors and limiting them to those who live in your household.
– Wearing a cloth face mask when out in public.
– Washing hands with soap and water for a minimum of 20 seconds.
– Avoiding touching eyes, nose or mouth with unwashed hands.
– Covering a cough or sneeze with your sleeve, or disposable tissue. Wash your hands afterward.
– Avoiding close contact with people who are sick.
– Staying away from work, school or other people if you become sick with respiratory symptoms like fever and cough.
– Following guidance from public health officials.
Always check with trusted sources for the latest accurate information about novel coronavirus:
– Los Angeles County Department of Public Health
– California Department of Public Health
– Centers for Disease Control and Prevention
– Spanish
– World Health Organization
L.A. County residents can also call 2-1-1.
What to Do if You Think You’re Sick
Call ahead: If you are experiencing symptoms of COVID-19 (fever, cough or shortness of breath), call your health care provider before seeking medical care so that appropriate precautions can be taken. More than 85 community testing sites also offer free, confidential testing: Find a COVID-19 Testing Site.
For more information about what Californians can do to prevent the spread of COVID-19, visit Coronavirus (COVID-19) in California.
California continues to issue guidance on preparing and protecting California from COVID-19. Consolidated guidance is available on the California Department of Public Health’s Guidance webpage.
Like this:
Like Loading...
Related




 Tweet This
Tweet This Facebook
Facebook Digg This
Digg This Bookmark
Bookmark Stumble
Stumble RSS
RSS



























REAL NAMES ONLY: All posters must use their real individual or business name. This applies equally to Twitter account holders who use a nickname.
0 Comments
You can be the first one to leave a comment.