 War is being waged on behalf of American citizens against the business takeover of hospitals, yet most people don’t realize this battle exists. Surprisingly, the warriors scattered throughout our country in this fight are doctors.
War is being waged on behalf of American citizens against the business takeover of hospitals, yet most people don’t realize this battle exists. Surprisingly, the warriors scattered throughout our country in this fight are doctors.
Unlike recent scandalous headlines of Wells Fargo committing fraud against its customers, Mylan’s heinous price gouging for its EpiPen and oil company disasters like the Deepwater Horizon, hospitals have created a shield against criticism by using a mantra that they are “too important to fail.” Touting this defense, hospital administrators have self-aggrandized their position and covertly bestowed profits, enriching personal salaries, bonuses and golden parachutes while the public is left to suffer.
Healthcare in our country is in shambles. As a geriatric physician, I have seen my elder patients targeted, pushing them into nursing homes, onto hospice and quickly pulling the plug, declaring them brain dead. These tactics, though, are part of a wider conspiracy among business people and lawyers who 20 years ago developed a game plan to capitalize on a disarrayed system. Being at a small community non-profit hospital allowed recognition of their strategic template.
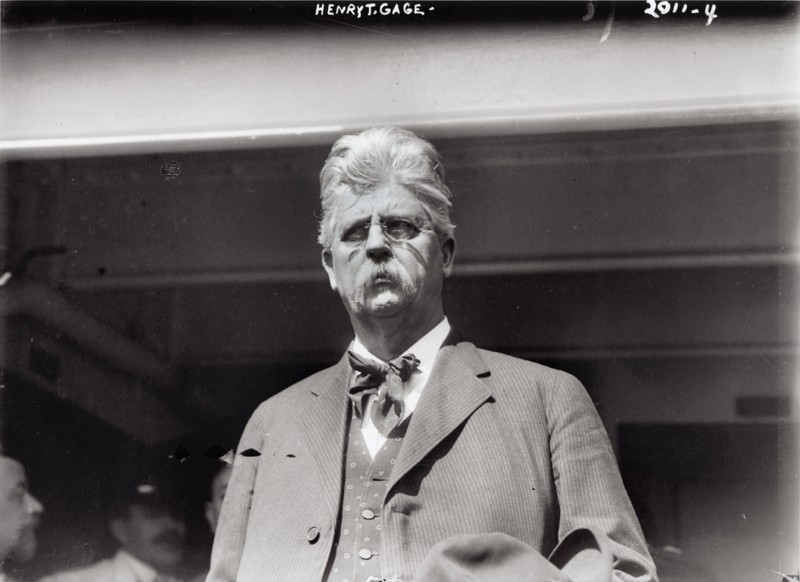
In the past decade, legal rights of the physician medical staff at Henry Mayo Newhall Hospital have been overrun, using “divide and conquer” tactics awarding favored doctor stipends for hospital directorships and signing contracts with chosen medical groups. Thereafter, MD votes on the board and certain committees were used against whistleblowing doctors who were punished or eliminated from staff. Subsequently, poor hospital performance statistics were hidden or manipulated while doctor input insuring quality care was ignored. This continues today.
Public awareness is minimal, as local media and politicians have hospital advertisement dollars and campaign funding dangled in their faces. Likewise, regulatory agencies like the Joint Commission, Department of Public Health, Medicare (CMS), and the state attorney general have succumbed to the “too important to fail” mantra with the proverbial “slap on the hand” punishment. (The same we will see with Wells Fargo, Mylan and, of course, oil companies.)
Doctors are now a profitable commodity controlled by businesses that shape physician decision-making through monetary influence or threat. Because of this, very few doctors at our hospital were willing to step forward, so former Chief of Staff Dr. Gregory Jenkins and I reached out for help.
A colleague from Let My Doctor Practice, Dr. Michael Strickland, referred us to a group in San Francisco, Physicians Organizing Committee (POC), led by Geoff Wilson. Our visit to their office earlier this year gave us insight into their 33 years of experience in this doctor struggle.
That same week, Dr. Jenkins heard the entire physician Medical Executive Committee (MEC) of Tulare Regional Medical Center was illegally ousted by the Board of Directors. In common with Henry Mayo doctors was a nonprofit hospital in a small community, building a “tower” for more patient beds, and both opened a for-profit membership gym. Coincidence or template?
Contacts were made, and the POC deftly launched a counter-offensive, legally and publicly. Rallies and community meetings pushed physician problems into the political forefront, and although the battle is ongoing, victories have been achieved.
For Dr. Jenkins and myself, this gave us hope.
Survival of our hospital is critical, as it went through bankruptcy 15 years ago, and the emotional fear still lingers. Santa Clarita is a growing community in an isolated valley, and we have only one hospital to serve us. Its loss would be detrimental to our citizens, especially elder seniors. Hospital administrators strategically remind the public and regulatory agencies of their past plight, generating fear that denudes scabs off of old wounds. Fear, though, cannot be an excuse for poor patient care.
The CEO is a recent past president of the California Hospital Association. Thus he knows the business template well and has harnessed it against the Henry Mayo physician medical staff.
As background, doctors at all hospitals in California are given the right of self-governance, legally separating them from the administration and Board of Directors. These laws are specifically made to safeguard the public from unscrupulous business people who might scheme to augment profits while providing cut-rate care. Physicians therefore cannot be employed by a hospital, preventing manipulation of medical decision-making through threats against salaries, bonuses, raises and tenure.
But hospitals have lawyers always looking for loopholes, so because they cannot directly hire doctors, they instead appoint them to paid hospital positions as directors; sign contracts with medical groups; or provide “loan” money to open and sustain a practice. These physicians become subservient to the hospital board and administration and succumb to the same manipulations self-governance should protect. Loophole.
The Henry Mayo Hospital Board of Directors has been financially conflicted by the administration, so their influenced vote is used to encroach physician self-governance. Here are some examples:
Recently the administration made a false claim against the MEC of impeding approval of physician assistants (PAs). In violation of state law, the board independently approved PAs who were allowed to care for critically ill patients throughout the hospital. Some PAs approved by the board were found not to be qualified to practice in our hospital, exposing extremely ill patients to subordinate care.
The administration-run Palliative Care Committee created a policy allowing non-physicians to consult the team. This is a medical decision that should be made only by doctors, as the consequence of this determination may lead to end-of-life hospice care. Allowing arbitrary medical decision-making forced vulnerable patients out of the hospital, inflating profits.
The Board of Directors enabled administrators to change the hospital Sentinel Event Policy, likely contributing to the death of a patient. When someone dies or is severely injured, some of these cases should be investigated. Originally, the policy directed the physician chief of staff to make the determination designating the case a “sentinel event,” launching an inquiry. But instead, administrators changed the policy and removed physician authority to make this decision, putting it into the hands of – guess who? – the administration.
There have been many more assaults encroaching on physician self-governance against the MEC, medical staff, and individual doctors. So far, we have seen only superficial corrections ordered by regulatory agencies. Why? For fear it might close or bankrupt the hospital?
Freeing hospitals from accountability when patients die or their lives are put in jeopardy only allows the problem to perpetuate. More dangerous in this business world, hospitals have joined Wells Fargo, Mylan and oil companies in their scandalous attempt to deceive the public.
Warfare must be sustained through proactive doctor groups like the Physicians Organizing Committee and the rising voices being heard through online blogs. Healthcare may be in shambles, but doctors and the public need to organize and coalesce in addressing this threat. There is hope, so we can’t give up the fight.
I’m not an historian and will be happy to be corrected, but an inspirational fact that stood out from high school history class is Gen. George Washington fought nine major battles during the Revolution. He lost seven … but still won the war.
Gene Uzawa Dorio, M.D., is a housecall geriatric physician and member of the Physicians Organizing Committee at Henry Mayo Newhall Hospital. The views expressed in this column as his alone. This commentary appears in the Fall edition of New Diagnosis .
Like this:
Like Loading...
Related







 Tweet This
Tweet This Facebook
Facebook Digg This
Digg This Bookmark
Bookmark Stumble
Stumble RSS
RSS





































REAL NAMES ONLY: All posters must use their real individual or business name. This applies equally to Twitter account holders who use a nickname.
1 Comment
Wow, this is an important war on healthcare in our country. I’m glad to hear there are some physicians to whom quality of care and the human side of patient care still matters. I have know a hospital administrator or two and when talking with them – they always came across as self-serving and full of bull. Never a definitive answer but fear mongering always ended the conversation. The fear mongering seemed to float down to their closest staff also, ie messages along the line of if you keep questioning…. Not saying all hospital administrators are like that, just the ones I’ve encountered.