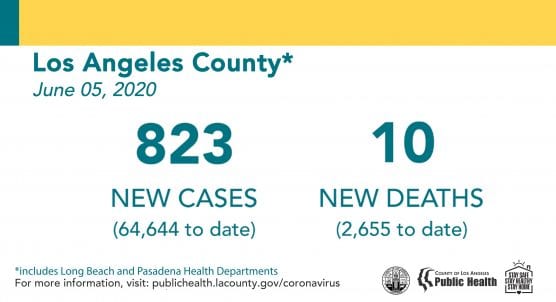
Note: The L.A. County graphic above is incorrectly dated June 5, and should be dated June 8. The graphic’s other information is accurate.
The Los Angeles County Department of Public Health on Monday confirmed 823 new cases of COVID-19 and 10 new deaths due to the virus countywide, with a total of 2,228 cases reported in the Santa Clarita Valley since the pandemic began, 25 more than reported Sunday.
The decrease in cases and deaths may reflect a reporting lag from over the weekend, Public Health officials said Monday.
In the SCV, 22 people have died of the virus to date — 18 resided in the city of Santa Clarita, 1 in Acton, 1 in Castaic, 1 in unincorporated Valencia and 1 in unincorporated Bouquet Canyon.
Countywide, Public Health has reported 64,644 positive cases of COVID-19 and a total of 2,655 deaths to date. Ninety-three percent of people who died had underlying health conditions.
Statewide, the California Department of Public Health has reported a total of 131,319 confirmed cases and 4,653 deaths from COVID-19 as of June 6. Currently, there are 3,184 confirmed hospitalizations and 1,079 ICU hospitalizations.
As of June 7, local health departments have reported 11,111 confirmed positive cases in healthcare workers and 66 deaths statewide.

Santa Clarita Valley Monday Update
Of the 2,228 cases reported to Public Health for the SCV to date, the community breakdown is as follows:
City of Santa Clarita: 846
Castaic: 1,239 (includes Pitchess Detention Center and North County Correctional Facility*)
Canyon Country (unincorporated portion): 36
Stevenson Ranch: 36
Val Verde: 29
Acton: 13
Agua Dulce: 10
Valencia (unincorporated portion west of I-5): 9
Saugus (unincorporated portion): 4
Elizabeth Lake: 3
Bouquet Canyon: 1
Lake Hughes: 1
Newhall (Unincorporated portion): 1
*Note: The county is not able to break out separate numbers for Castaic and the PDC/NCCF because the county uses geotagging software that is not easy to change, according to county spokesperson Stephanie English. Click here for the LASD COVID-19 dashboard.

Henry Mayo Monday Update
Henry Mayo Newhall Hospital reported its 11th COVID-related death on Wednesday, June 3, according to hospital spokesman Patrick Moody.
Eleven of the SCV’s 22 fatalities to date have occurred at Henry Mayo.
As of Wednesday, of the 1,824 persons tested at Henry Mayo to date, 227 tested positive, 1,810 were negative, 17 were pending and 8 patients were hospitalized in a dedicated unit receiving ICU-level care. A total of 84 COVID-19 patients have been discharged so far.
Discrepancies in the testing numbers are due to some patients being tested more than once, he said.
The hospital is now releasing numbers on a weekly basis (Wednesdays), unless there is a drastic change in the number of cases or a death has been confirmed, Moody said.

L.A. County Demographics
Six people who died were over the age of 65 years old and three people who died were between the ages of 41 and 65 years old. Five people had underlying health conditions including three people over the age of 65 years old and two people between the ages of 41 to 65 years old. One death was reported by the City of Pasadena.
Of those who died, information about race and ethnicity is available for 2,463 people (99 percent of the cases reported by Public Health) 41% of deaths occurred among Latino/Latinx residents, 28% among White residents, 18% among Asian residents, 12% among African American residents, 1% among Native Hawaiian/Pacific Islander and residents identifying with other races.
Upon further investigation, 23 cases reported earlier were not L.A. County residents.
Public Health continues to track disproportionality in health outcomes by race, ethnicity and income level data of people who have been tested, hospitalized and died from COVID-19.
African Americans, Native Hawaiian/Pacific Islanders, and people living in communities with high levels of poverty continue to have the highest rate of death per 100,000 people for COVID-19 when compared to other groups.
Native Hawaiian/Pacific Islanders have a death rate of 30 per 100,000, African Americans have a death of 31 per 100,000, Latinos/Latinxs have a death of 29 per 100,000, Asians have a death rate of 21 per 100,000, and Whites have a death rate of 15 per 100,000.
People who live in areas with high rates of poverty have almost four times the rate of deaths for COVID-19 with 51 per 100,000 people, compared with communities with very low poverty levels who had a death rate of 13 per 100,000.
Public Health continues collaboration with community, healthcare, and philanthropic partners to improve testing, connection to care and services, and in-language and culturally appropriate communications to the communities experiencing these inequitable outcomes.

“Every day, we report these numbers knowing that they represent real people who have passed away, and they represent families and friends who are experiencing profound loss,” said Barbara Ferrer, PhD, MPH, MEd, Director of Public Health. “Our thoughts and prayers are very much with you all. We are so sorry for your loss.
“Every social interaction outside the household comes with risk to both the people who interact and, if anyone gets infected, to the people they live, work and play with in the future,” Ferrer said. “Please take time to take common-sense precautions to reduce the risk of infecting others and/or becoming infected.”
L.A. County Healthcare Workers
Public Health continues tracking the number of positive cases and deaths among healthcare workers related to the COVID-19 pandemic response.
Public Health has confirmed 41 people who died from COVID-19 worked in a healthcare setting; 29 people who died worked in skilled nursing and assisted living facilities, six people worked in hospitals, two people worked in home health, one person worked in a correctional facility, one person worked in a laboratory, and one person worked in an outpatient facility.
For one health care worker who passed away, their workplace setting is not specified. A total of 6,031 confirmed cases of COVID-19 occurred among healthcare workers and first responders; this is an additional 633 new cases reported since the previous week. Seven percent of healthcare workers with COVID-19 have been hospitalized.
Forty-four percent of cases are among nurses, though cases have been identified among a range of occupational roles, including caregivers, people who work in administration, physicians and medical assistants.
Sixty percent of these cases reported a known source of exposure, and 79% of healthcare workers with known exposure reported being exposed in a healthcare facility.
Healthcare workers who are positive worked at 27 different occupational settings, with the vast majority of cases among healthcare workers from skilled nursing facilities and hospitals.

L.A. County Testing
As of Monday, 6,923 people who tested positive for COVID-19 (11% of positive cases) have been hospitalized at some point during their illness. There are 1,399 people who are currently hospitalized, 30% of these people are in the ICU and 21% are on ventilators. Testing capacity continues to increase in L.A. County, with testing results available for over 708,000 individuals and 8% of people testing positive.
COVID-19 testing is prioritized for hospitalized patients, healthcare workers, and first responders with symptoms, as well as residents and employees, both symptomatic and asymptomatic, in long-term care facilities or other congregate living settings where there are outbreaks.
Additionally, Public Health recommends testing for anyone who is older or has underlying health conditions with symptoms, as well as people who have been close contacts of people who are positive for COVID-19. Anyone with symptoms should consider testing as well.
Testing negative for COVID-19 right after being exposed does not mean you can’t become infected later during the incubation period. Individuals who are tested too soon after being exposed, are less likely to test positive because their viral load may be undetectable to the test.
If anyone was possibly exposed to someone with COVID-19, and the test result is negative, they should remain at home for 14 days to prevent spreading illness to others.
COVID-19 testing is prioritized for hospitalized patients, healthcare workers, and first responders with symptoms, as well as residents and employees, both symptomatic and asymptomatic, in long-term care facilities or other congregate living settings where there are outbreaks.
Additionally, Public Health recommends testing for anyone who is older or has underlying health conditions with symptoms, as well as people who have been close contacts of people who are positive for COVID-19.
Anyone with symptoms should consider testing as well. For more information on how to get tested, visit covid19.lacounty.gov/testing.

Best Protections
Because COVID-19 is still relatively easy to transmit and continues to cause serious illness and death, everyone should always wear a face covering securely over their nose and mouth and keep six feet apart from others not in their household when out and about.
Businesses must continue to implement their physical distancing and infection control protocols that protect both employees and customers.
If anyone has been in a crowded setting, where people are congregating who are not using face coverings or distancing, or if you had close contact (within 6 feet for greater than 15 minutes) with non-household members who were not wearing face coverings please consider the following:
* If you live with persons who are elderly or have high-risk conditions, you should also maintain a six-foot distance and wear a face covering when you are with them at home, avoid preparing food for others, sharing utensils, bedding and towels, and increase cleaning and disinfecting of common surfaces.
* Consider getting tested for COVID-19 if you have been exposed to someone that is positive or likely positive.
The best protection against COVID-19 continues to be to wash your hands frequently, avoid touching your eyes, nose, and mouth with unwashed hands, self-isolate if you are sick, practice physical distancing and wear a clean face covering when in contact with others from outside your household.
People who have underlying health conditions remain at much greater risk for serious illness from COVID-19, so it will continue to be very important for the county’s vulnerable residents to stay at home as much as possible, to have groceries and medicine delivered, and to call their providers immediately if they have even mild symptoms.
The L.A. County Safer at Work and in the Community Health Officer Order, Reopening Protocols, COVID-19 Surveillance Interactive Dashboard, Roadmap to Recovery, Recovery Dashboard, and additional things you can do to protect yourself, your family and your community are on the Public Health website, www.publichealth.lacounty.gov.
Here’s the county’s incident report for Monday, June 8:
[Open .pdf in new window]

California Demographics
Overall, for adults 18 and older, Latinos, African Americans and Native Hawaiians and Pacific Islanders are dying at disproportionately higher levels. The proportion of COVID-19 deaths in African Americans is about double their population representation across all adult age categories.
For Native Hawaiians and Pacific Islanders, overall numbers are low, but there is nearly a four-fold difference between the proportion of COVID-19 deaths and their population representation. More males are dying from COVID-19 than females, in line with national trends.
More information is available at COVID-19 Race and Ethnicity Data.
Testing in California
As testing capacity continues to increase across the state, the California Department of Public Health is working to expand access to COVID-19 testing. Testing should be used for medical evaluation of persons with symptoms of COVID-19 as well as for efforts by public health agencies and essential employers to prevent and control the spread of COVID-19.
As of June 7, there have been 2,431,190 tests conducted in California and reported to the CDPH, an increase of 68,972 tests over the prior 24-hour reporting period.
These numbers include data from commercial, private and academic labs, including Quest, LabCorp, Kaiser, University of California and Stanford, and the the 25 state and county health labs currently testing.
More than 85 community testing sites also offer free, confidential testing: Find a COVID-19 Testing Site.

New Data Portal
The state has launched a new, user-friendly data portal at COVID-19 Statewide Update that tracks COVID-19 cases statewide and by county, gender, age and ethnicity. The portal also outlines statewide hospitalizations and testing efforts. The data presented on the portal will be updated daily and will include additional information as it is available.
What to Do if You Think You’re Sick
Call ahead: If you are experiencing symptoms of COVID-19 (fever, cough or shortness of breath), call your health care provider before seeking medical care so that appropriate precautions can be taken. More than 85 community testing sites also offer free, confidential testing: Find a COVID-19 Testing Site.
For more information about what Californians can do to prevent the spread of COVID-19, visit Coronavirus (COVID-19) in California.
California continues to issue guidance on preparing and protecting California from COVID-19. Consolidated guidance is available on the California Department of Public Health’s Guidance webpage.
Like this:
Like Loading...
Related




 Tweet This
Tweet This Facebook
Facebook Digg This
Digg This Bookmark
Bookmark Stumble
Stumble RSS
RSS
































REAL NAMES ONLY: All posters must use their real individual or business name. This applies equally to Twitter account holders who use a nickname.
0 Comments
You can be the first one to leave a comment.