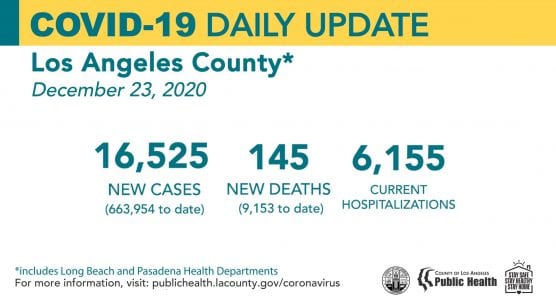
The Los Angeles County Department of Public Health on Wednesday again reported the highest number of new COVID-19 deaths and hospitalizations ever reported in a single day since the pandemic began, as Henry Mayo Newhall Hospital in Valencia reported its 60th COVID fatality.
Public Health confirmed 145 new deaths and 16,525 new cases of COVID-19 countywide — one of the highest number of new cases ever reported — and 6,155 people with COVID-19 are currently hospitalized, 20% of them in the ICU.
“Two-thirds of these patients are suffocating due to the inflammation that’s in their lungs that’s caused by the virus,” said L.A. County Health Director Dr. Christina Ghaly. “They’re suffocating to the point where they can no longer breathe on their own and they have to have someone put a tube down their throat in order to oxygenate their organs. Many of these people will not live to see 2021.”
The Santa Clarita Valley has now tallied 14,780 confirmed COVID-19 cases among residents – 389 more new cases since Tuesday – and 104 deaths, according to the latest Public Health data, which does not yet include the death reported today by Henry Mayo.
To date, Public Health identified 663,954 positive cases of COVID-19 across all areas of L.A. County and a total of 9,153 deaths.
“For those missing their loved ones who have passed, we extend our deepest sympathies for your loss and wish you peace this holiday,” said Barbara Ferrer, PhD, MPH, MEd, Director of Public Health.
The COVID-19 surge is having a devasting impact on L.A. County. In September, when the number of new cases remained fairly flat, the rate of hospitalizations and deaths were relatively low. Once the county began experiencing this surge in early November, the daily number of hospitalizations and deaths increased just as quickly.
In order for hospitalizations and deaths to decrease, cases need to start going down.

“Tragically, we are on our way to witnessing 10,000 deaths from COVID-19 and our hospitals overwhelmed with COVID-19 patients,” Ferrer said. “Every day, more than 14,000 additional people become intimately aware of the easy spread of this virus because they test positive for COVID-19.
“The winter holidays invite us to spread joy and light to those around us,” she said. “Perhaps as we weigh the request to delay travel plans and gather only with members of our household, we can find comfort in making these sacrifices because we know that by staying home, we are giving others the ultimate holiday gift: we may be saving their lives.
“We are in the middle of a horrific surge and we all need to take the hard steps, the wise steps, to reduce transmissions and exposure now, during the holidays, and as we begin 2021,” she said. “The sooner we all take these vitally important steps, the sooner we can stop the surge in cases that is overwhelming our hospital care system.”
“Anyone who is willing to be honest with the facts and the timeline of the rising case counts and the reality that is bombarding our hospitals must accept that our collective behaviors as a community of Los Angeles County in the days around Thanksgiving directly led to our rising rate of hospitalization and our rising rate of death,” Ghaly said.
“Images of crowded, outdoor malls and jam-packed parking lots, of people sitting to eat with other people, people taking walks without masks, playgrounds with kids and parents who don’t have their masks on, or who are sipping coffee with their masks off with other people close by” are just some of the examples Ghaly listed in answer to a question about lack of public cooperation with public health orders.
See more SCV and L.A. County info later in this report.

California Wednesday Snapshot
Statewide, as of Tuesday, December 22, the California Department of Public Health confirmed a total of 1,964,076 COVID-19 cases (up 39,069), with 23,284 deaths from the disease (up 361) since the pandemic began.
There are 18,448 confirmed hospitalizations and 3,827 ICU hospitalizations in the state, continuing a very sharp upward trend.
The 7-day positivity rate is 12.6% and the 14-day positivity rate is 12.3.0%, showing a slightly lower trend.
As of December 22, local health departments have reported 64,959 confirmed positive cases in health care workers and 244 deaths statewide.
There have been 30,468,560 tests conducted in California, an increase of 278,378 over the prior 24-hour reporting period.
Numbers do not represent true day-over-day change as these results include cases from prior to yesterday.
See more California information later in this report.

Screencap from the Johns Hopkins University’s Center for Systems Science and Engineering COVID-19 dashboard, showing COVID cases in the United States as of Wednesday afternoon, December 23, 2020.
Worldwide Infections Top 78 Million People; U.S. Deaths Top 325,000
Worldwide, 78,471,775 people have been infected by COVID-19 while 1,725,959 people have died of the virus as of 1:22 p.m. Wednesday Pacific Time, according to data compiled by Johns Hopkins University.
In the U.S., more than 18,381,991 Americans have been diagnosed with COVID-19. New cases and hospitalizations continue at all-time record highs. The number of people in the U.S. who have died due to the virus has now surpassed 325,097.
With 4.25% of the world’s population (328.2 million) and more than 20% of the confirmed COVID-19 cases, the U.S. also continues to lead the world in deaths.
By comparison, Brazil (population 209.5 million) is No. 2 in deaths with 188,259, and No. 3 in cases with 7,318,821 India (population 1.353 billion) is No. 2 in cases, with 10,099,066 confirmed cases and 146,444 deaths as of Wednesday afternoon.
Henry Mayo Newhall Hospital Wednesday Update
After reporting its 58th and 59th COVID-caused deaths on Monday, Henry Mayo Newhall Hospital reported its 60th COVID fatality on Wednesday, spokesman Patrick Moody said.
In the month of November, 8 COVID-19 patients died at Henry Mayo. In December, as of Dec. 23, with 8 days left in the month, 24 people had died at the hospital, Moody said, an average of more than one death per day.
As of Wednesday, of the 14,605 people tested for COVID-19 at Henry Mayo to date, 2,148 tested positive, 17,493 were negative, 1 was pending, 90 patients were hospitalized in a dedicated unit receiving ICU-level care (an increase of 6 since Monday), and a total of 590 COVID-19 patients have been treated and discharged so far.
Discrepancies in the testing numbers at the hospital are due to some patients being tested multiple times, Moody said.
Henry Mayo releases complete statistics weekly, usually on Wednesdays, unless a new death occurs, he said.
Privacy laws prohibit the hospital from releasing the community of residence for patients who die there; that info is reported by the L.A. County Public Health COVID-19 dashboard, which is generally 48 hours behind.

Santa Clarita Valley Wednesday Update
As of 8 p.m. Monday, December 21, the latest update to the L.A. County Public Health COVID-19 data dashboard, 104 deaths had been reported among Santa Clarita Valley residents since the pandemic began, not including the death reported Wednesday by Henry Mayo.
Of the 105 SCV residents who have died, 86 lived in Santa Clarita, 5 in Castaic, 5 in Stevenson Ranch, 3 in Acton, 1 in unincorporated Bouquet Canyon, 3 in unincorporated Canyon Country, and 1 in Val Verde, according to the data dashboard, plus 1 in a community not yet named.
Of the 14,780 confirmed COVID-19 cases reported to Public Health for the SCV to date, the community breakdown is as follows:
City of Santa Clarita: 10,204
Castaic: 2,792 (includes Pitchess Detention Center and North County Correctional Facility*)
Stevenson Ranch: 522
Canyon Country (unincorporated portion): 433
Acton: 225
Val Verde: 153
Agua Dulce: 113
Valencia (unincorporated portion west of I-5): 95
Saugus (unincorporated portion): 72
Newhall (Unincorporated portion): 51
Elizabeth Lake: 36
Lake Hughes: 21
Saugus/Canyon Country: 21
Bouquet Canyon: 22
Sand Canyon: 8
San Francisquito/Bouquet Canyon: 4
*Note: The county is unable to break out separate numbers for Castaic and PDC/NCCF because the county uses geotagging software that cannot be changed at this time, according to officials. Click here for the LASD COVID-19 dashboard.

Martin Reyes, RN for the Intensive Care Unit at LAC+USC Medical Center, receives a COVID-19 vaccination on Dec. 18 as part of L.A. County Health Services’ effort to vaccinate more than 10,000 frontline healthcare workers by the end of 2020.
L.A. County Vaccine Update: Who Gets it When
Initial efforts are aimed at vaccinating everyone in Phase 1A, Tier 1; these are our frontline healthcare workers and residents in long-term care facilities. Looking ahead, once we are done with vaccinating all groups in Tier 1, we will move to Tier 2 and Tier 3.
In Phase 1A, Tier 2, this group includes healthcare workers in immediate care facilities and home healthcare service, community health workers, public health field staff, and healthcare workers in primary care clinics, correctional facility clinics, and urgent care clinics.
In Phase 1A, Tier 3, this group includes healthcare workers in specialty clinics, laboratory workers, dental and other oral health clinics, and pharmacy staff who are not within the higher-tier settings.
As county health officials begin with the first set of vaccinations for all the Tiers within Phase 1A, we can begin to look at categories of individuals to receive vaccinations under Phase 1B and 1C. These are Phases adopted by the CDC to assist prioritization while there is a limited supply of the vaccine and we’re following their guidance.
Persons within Tier 1B are considered persons 75 years and older and frontline essential workers. These include firefighters, police officers and sheriff’s deputies, teachers and school staff, manufacturing workers, corrections workers, U.S. Postal Service workers, public transit and grocery store workers. A complete list will be published online.
Persons within Tier 1C are those who are 65 years or older and individuals 16 years and older with significant underlying health conditions that could create a serious health risk. This also includes additional essential workers not included in Tier 1B.
For more information about the county’s vaccination plans, visit www.publichealth.lacounty.gov.
While the news about cases, hospitalizations and deaths remains very alarming, there is significant hope on the horizon with the start of vaccinations in L.A. County. Public Health is collecting data from the 83 acute care hospitals, where frontline healthcare workers are receiving vaccinations, as well as from the teams who are going out to skilled nursing facilities to administer vaccines to the healthcare workers and residents.

As of Tuesday night, more than 38,800 frontline healthcare workers have been vaccinated at acute care hospitals with the Pfizer vaccine. Our first two shipments of the Pfizer vaccine include 131,600 doses. We also received our first shipments of the Moderna vaccine and are distributing the 116,600 doses this week at skilled nursing facilities and to EMTs and firefighters.
Public Health created a COVID-19 vaccine management dashboard that will be updated weekly to list how many vaccine allocations have been received and where they have been distributed. This dashboard will also provide a running tally of how many doses have been administered. Currently, this dashboard shows the vaccines being administered within Phase 1a where frontline healthcare and public health workers in hospitals, healthcare facilities, clinics, labs, and field settings are vaccinated along with staff and residents at long-term care facilities and frontline EMTs and paramedics.
For more information, visit www.publichealth.lacounty.gov.
More L.A. County Demographics: Age
Of the 145 new deaths reported today, 55 people who died were over the age of 80 years old, 36 people who died were between the ages of 65 and 79 years old, 30 people who died were between the ages of 50 and 64 years old, six people who died were between the ages of 30 and 49 years old, and one person who died was between the ages 18 and 29 years old.

One hundred and six people who died had underlying health conditions including 49 people over the age of 80 years old, 28 people between the ages of 65 and 79 years old, 22 people between the ages of 50 and 64 years old, five people between the ages of 30 and 49 years old, and one person between the ages of 18 and 29 years old.
Hypertension, high cholesterol, obesity, and diabetes are the most common underlying health conditions among people hospitalized with COVID-19. Many people have multiple underlying health conditions.
Fourteen deaths were reported by the City of Long Beach and one death was reported by the City of Pasadena.
Cases by Age Group (Los Angeles County only — excluding Long Beach and Pasadena)
Young people are continuing to drive the surge of the virus’s community spread with disastrous results for our elderly.
* 0 to 4: 12110
* 5 to 11: 28220
* 12 to 17: 34697
* 18 to 29: 154794
* 30 to 49: 214610
* 50 to 64: 119299
* 65 to 79: 45917
* over 80: 17552
* Under Investigation 4226

More L.A. County Demographics: Race/Ethnicity
As the COVID-19 pandemic worsens, the gaps between race and ethnicity groups that the county made progress closing in September continue to widen, particularly for Latino/Latinx residents compared to other groups, though all groups are experiencing increases.
Latino/Latinx residents are now seeing a 7-day cumulative rate of nearly 650 new cases per 100,000 people. This is more than two times that of African American/Black residents, the group with the second-highest case rate of about 270 new cases per 100,000 people, and almost three times the rate experienced by white residents (250 new cases per 100,000 people) and Asian residents (172 new cases per 100,000 people).
Latino/Latinx, African American/Black, and Asian residents are also experiencing an alarming increase in deaths. The death rate among Latino/Latinx residents has increased from 1.5 deaths per 100,000 people to 4.5 deaths per 100,000 people. The death rate for African American/Black residents has increased from less than 1 death per 100,000 people to 3 deaths per 100,000 people. The death rate among Asian residents has increased from 0.5 deaths per 100,000 people to 3 deaths per 100,000 people.
Public Health continues to see a high mortality rate among people living in areas with the highest levels of poverty, with four times the death rate compared to people living in the lowest levels of poverty.
Throughout the pandemic, the life and death consequences of racism and poverty have played out in devastating ways and they continue to do so. The widening gaps are a stark reminder that many of our essential workers are Black and brown, and many are not able to telework or stay home; many work at jobs with low wages, and live in under-resourced neighborhoods.
During the surge, all our essential workers are taking on increased risks at their jobs because community transmission rates are high. The only way to reduce their risk is for every business to fully implement the safety modifications required by the Health Officer Order; this includes providing appropriate PPE and infection control. Violations at workplaces can be reported anonymously at 888-700-9995.
Every resident needs to protect our essential workers by playing by rules. This means always wear a face covering and keep distance from others, no crowding, frequent handwashing, and limiting all non-essential activities.
Test Positive? Isolate, Contact Trace
It is important to isolate if you tested positive for COVID-19 for 10 days and to self-quarantine for 10 days if you have come in contact with someone who tested positive for COVID-19. L.A. County has capacity to support isolation and quarantine for those who are positive and those who are close contacts.
If you are positive for COVID-19 and need help figuring out how to best stay away from others for the 10 days, please answer the call when Public Health contacts you or call Public Health at 833-540-0473.
L.A. County Public Health’s Reopening Protocols, COVID-19 Surveillance Interactive Dashboard, Roadmap to Recovery, Recovery Dashboard, and additional things you can do to protect yourself, your family and your community are on the Public Health website, www.publichealth.lacounty.gov.

Vaccinate All 58
The COVID-19 shipment of the COVID-19 vaccine has arrived in California, and additional shipments will continue to arrive throughout this week. The first doses are being administered to health care workers and residents of long-term care facilities. The state is working closely with community partners and stakeholders to help ensure the vaccine is distributed and administered equitably across California.
For more information, visit the CDPH COVID-19 Vaccine webpage and Vaccinate All 58.
California Regional Stay Home Order
Due to high rates of COVID-19 hospitalizations impacting the health care system, California is under a Limited Stay at Home Order. The order applies to all counties that are currently under the Regional Stay at Home Order and those in Tier One (Purple) of the Blueprint for a Safer Economy.
The Limited Stay at Home Order will expire after the Regional Stay Home Order has been terminated in all regions of the state.
Based on ICU data, four regions, San Joaquin Valley, Southern California, Greater Sacramento and the Bay Area are under the Regional Stay at Home Order as of Wednesday, Dec. 23.
Regions must remain under the Regional Stay at Home Order for at least three weeks and will be eligible to exit the order and return to the Blueprint for a Safer Economy only if ICU capacity projections for the following month are above or equal to 15%.
Current available ICU capacity by region:
* Bay Area: 13.7%
* Greater Sacramento Region: 16.2%
* Northern California: 28.7%
* San Joaquin Valley: 0.0%
* Southern California: 0.0%

San Joaquin Valley and Southern California will be eligible to exit from the order and return to the Blueprint for a Safer Economy on December 28 if ICU capacity projections for the following month are above or equal to 15%. Greater Sacramento may exit on January 1 and the Bay Area on January 8 if both achieve the same capacity projections.
The state continues to support hospital systems and congregate care facilities across the state as ICU capacity continues to drop. The state is providing staff assistance, personal protective gear, durable medical equipment and supplies, and infection prevention technical assistance.
On Sunday, December 13, CDPH implemented a temporary waiver of nurse-to-patient ratios for intensive care units, step-down units, emergency medical services and medical and surgical units. In addition, more than 300 additional medical staff has been deployed across the state, with more expected before the end of the month.
Read the full Regional Stay Home Order and Supplement to the Order, and Frequently Asked Questions.

California Blueprint for a Safer Economy
Governor Gavin Newsom’s Blueprint for a Safer Economy imposes risk-based criteria on tightening and loosening COVID-19 allowable activities and expands the length of time between changes to assess how any movement affects the trajectory of the disease.
Californians can go to covid19.ca.gov to find out where their county falls and what activities are allowable in each county.
California Testing
More than 85 community testing sites offer free, confidential testing: Find a COVID-19 Testing Site.
The testing turnaround dashboard reports how long California patients are waiting for COVID-19 test results. California has worked to reduce testing turnaround times in recent weeks to help curb the spread of the virus.
During the week of December 6 to December 12, the average time patients waited for test results was 1.8 days. During this same time period, 46% of patients received test results in one day and 75% received them within two days. The testing turnaround time dashboard (PDF) is updated weekly.
All four tiers in the Testing Prioritization Guidance originally dated July 14, 2020, have equal priority for testing.
California Demographics
Overall, for adults 18 and older, Latinos, African Americans, and Native Hawaiians and Pacific Islanders are dying at disproportionately higher levels.
The proportion of COVID-19 deaths in African Americans is more than one-and-a-half times their population representation across all adult age categories. For Native Hawaiians and Pacific Islanders, overall numbers are low but almost double between the proportion of COVID-19 deaths and their population representation.
More males are dying from COVID-19 than females, in line with national trends.
More information is available at COVID-19 Race and Ethnicity Data.

Multisystem Inflammatory Syndrome in Children (MIS-C)
Each week, the California Department of Public Health updates the number of cases of Multisystem Inflammatory Syndrome in Children (MIS-C) reported in the state.
As of December 21, 157 cases of MIS-C have been reported statewide, an increase of 5 over the previous week. To protect patient confidentiality in counties with fewer than 11 cases, we are not providing total counts at this time.
MIS-C is a rare inflammatory condition associated with COVID-19 that can damage multiple organ systems. MIS-C can require hospitalization and be life-threatening. Parents should be aware of the signs and symptoms of MIS-C including fever that does not go away, abdominal pain, vomiting, diarrhea, neck pain, rash, bloodshot eyes, or feeling tired. Contact your child’s doctor immediately if your child has these symptoms. Early diagnosis and treatment of patients are critical to preventing long-term complications.

Protect Yourself and Your Family
California is experiencing the fastest increase in cases we have seen yet – faster than what we experienced at the outset of the pandemic and this summer. If COVID-19 continues to spread at this rate, it could quickly overwhelm our health care system and lead to catastrophic outcomes.
Protect yourself, family, friends, and community by following these prevention measures:
* Staying home except for essential needs/activities following local and state public health guidelines when patronizing approved businesses. To the extent that sectors are re-opened, Californians may leave their homes to work at, patronize, or otherwise engage with those businesses, establishments or activities.
* Following the limited Stay at Home Order that requires all non-essential work and activities to stop between 10 p.m. and 5 a.m. in counties in the purple tier. The order took effect at 10 p.m. Saturday, November 21, and will remain in effect until 5 a.m. December 21.
* Staying close to home, avoiding non-essential travel, and practicing self-quarantine for 14 days after arrival if you leave the state.
* Keeping gatherings small, short, and outdoors and limiting them to those who live in your household.
* Wearing a cloth face mask when out in public
* Washing hands with soap and water for a minimum of 20 seconds
* Avoiding touching eyes, nose, or mouth with unwashed hands
* Covering a cough or sneeze with your sleeve or disposable tissue. Wash your hands afterward
* Avoiding close contact with people who are sick
* Staying away from work, school, or other people if you become sick with respiratory symptoms like fever and cough
* Following guidance from public health officials
What to Do if You Think You’re Sick
Call ahead: If you are experiencing symptoms of COVID-19 (fever, cough or shortness of breath), call your health care provider before seeking medical care so that appropriate precautions can be taken. More than 85 community testing sites also offer free, confidential testing: Find a COVID-19 Testing Site.
It’s important if someone thinks they could be positive for COVID-19 and are awaiting testing results to stay at home and act as if they are positive. This means self-isolating for 10 days and 72 hours after symptoms and fever subside.
If a person tests positive for COVID-19, they should plan on receiving a call from a public health specialist to discuss how to protect themselves and others, find out where they may have been, and who they were in close contact with while infectious.

California COVID-19 Data and Tools
A wide range of data and analysis guides California’s response to COVID-19. The state is making the data and its analytical tools available to researchers, scientists and the public at covid19.ca.gov.
* The Statewide COVID-19 Dashboard
* The California COVID-19 Assessment Tool (CalCAT)
* State Cases and Deaths Associated with COVID-19 by Age Group
* COVID-19 Race & Ethnicity Data
* COVID-19 Hospital Data and Case Statistics
* View additional datasets at the California Open Data Portal (including Testing Data, PPE Logistics Data, Hospital Data, Homeless Impact and more)
Consolidated guidance is available on the California Department of Public Health’s Guidance webpage.
* * * * *
Always check with trusted sources for the latest accurate information about novel coronavirus (COVID-19):
* Los Angeles County Department of Public Health
* California Department of Public Health
* Centers for Disease Control and Prevention
* Spanish
* World Health Organization
* Johns Hopkins University COVID-19 Dashboard
L.A. County residents can also call 2-1-1.
* * * * *
Courthouse News Reporter Nathan Solis contributed to this report.
Like this:
Like Loading...
Related




 Tweet This
Tweet This Facebook
Facebook Digg This
Digg This Bookmark
Bookmark Stumble
Stumble RSS
RSS







































REAL NAMES ONLY: All posters must use their real individual or business name. This applies equally to Twitter account holders who use a nickname.
0 Comments
You can be the first one to leave a comment.