 Did you know that there are two different ways to receive your Medicare benefits?
Did you know that there are two different ways to receive your Medicare benefits?
The most popular way is Original Medicare. With Original Medicare, you can choose any doctor, hospital, or other healthcare provider you want, as long as they accept Medicare. When you receive medical services or goods, Medicare pays the provider directly.
The other way is Medicare Advantage, which is a form of managed care, like an HMO or PPO. Medicare Advantage plans are sold by private insurance companies approved by Medicare. If you’re in Medicare Advantage, you generally must go to doctors and other providers within the company’s network.
On the other hand, Medicare Advantage plans may cover some benefits – such as dental, hearing, and vision – that Original Medicare doesn’t.
Most people with Original Medicare pay a monthly premium. Some Medicare Advantage plans charge an additional monthly premium; others don’t.
With Original Medicare, you must pay deductibles and/or coinsurance when you get care.
To cover these “gaps” in Medicare, some people buy supplemental insurance called Medigap. If you have a Medigap policy, Medicare pays its share of the covered costs, and then your Medigap policy pays its share.
Original Medicare generally doesn’t cover prescription drugs. If you want drug coverage, you can purchase a Medicare Part D plan. Like Medicare Advantage, Part D plans are sold by private insurers, which charge a monthly premium for them.
About 70 percent of Medicare beneficiaries are currently in Original Medicare; the rest get coverage through Medicare Advantage.
Medicare Advantage companies must cover all of the services that Original Medicare covers, except hospice care and some care in qualifying clinical research studies. (Original Medicare covers these items even if you’re in a Medicare Advantage plan.)
Medicare Advantage plans cover emergency and urgent care, and many include some prescription drug coverage.
But the plans can charge different out-of-pocket amounts and they have different rules for how you get service.
For example, you may need a referral to see a specialist. And you may need to stay in their provider network, unless you’re willing to pay more to go outside the network.
You should always check with the plan before you get a service to find out whether it’s covered and what your costs may be. If the plan decides to stop participating in Medicare, you can join another Medicare health plan or return to Original Medicare.
How can you decide whether Original Medicare or Medicare Advantage is better for you?
There’s a more detailed explanation of the differences between Original Medicare and Medicare Advantage in the “Medicare & You” handbook, which is mailed to all Medicare households every fall. The handbook is also available through our website, www.Medicare.gov. (Go to “helpful links” at the bottom of the page.)
You can shop for a health or drug plan using the Medicare Plan Finder, also available on the Medicare.gov website. Click on the button that says, “Find health & drug plans.” (More about the new, improved Plan Finder in next month’s column.)
If you have any questions, you can always call Medicare’s toll-free number, 1-800-MEDICARE (1-800-633-4227). Customer service representatives are available 24/7.
If you’d like to join a Medicare Advantage or Part D drug plan, you can do so during Medicare’s open enrollment period, which runs from Oct. 15 to Dec. 7 each year.
If you’re in Original Medicare and you’re satisfied with it, you don’t need to do anything during open enrollment. But we find that people with Medicare Advantage or Part D plans can often save money by shopping around.
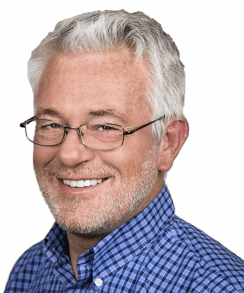
Greg Dill is Medicare’s regional administrator for Arizona, California, Nevada, Hawaii, and the Pacific Territories. You can always get answers to your Medicare questions by calling 1-800-MEDICARE (1-800-633-4227).
Like this:
Like Loading...
Related






 Tweet This
Tweet This Facebook
Facebook Digg This
Digg This Bookmark
Bookmark Stumble
Stumble RSS
RSS






































REAL NAMES ONLY: All posters must use their real individual or business name. This applies equally to Twitter account holders who use a nickname.
0 Comments
You can be the first one to leave a comment.